When we found out we were having a boy I was elated and mortified. The elation was due to the fact that we already had two beautiful little girls. Emma was two-years-old and Abby was one year. The closeness of age didn't scare me. When Abby came 13 months after Emma, I resigned myself to having children very close in age and being done bearing children by the time I was 30. No, what scared me to death was realizing that my baby was going to go under the knife for a circumcision. That scared me near to vomiting. Unfortunately, I had no idea how trivial that detail would become in my son's life.
During my pregnancy I was completing my sophomore year in college. I had been attending school for about a year after high school, but wanted more direction in my life than just taking a bunch of classes I had to pay for that may or may not contribute to my final degree. Instead, I took time off, got married to my best friend Josh, and we began having babies. Josh and I decided to go back to school not long after our second daughter, Abby, was born. We knew it would be difficult, but we also knew it was the only real option we had if we wanted to make a good life for our children. Josh was working on a biology degree and I thrived on my theatre degree. I acted in my first lead role while pregnant with Matthew. Luckily, I wasn't showing too much at that point. I made it through the spring semester without any real hiccups trying to balance home, school, and pregnancy, until right before finals week.
About three weeks left in the semester I saw my midwife for a checkup. I had been scheduled for an ultrasound because the one taken at 20 weeks didn't get a good look at Matthew's heart and kidneys. We sat through the ultrasound and joked around by asking if he were still a boy. Josh and I thought nothing of the extreme delay we experienced afterward as we waited for the midwife to give us the results of the ultrasound. We often waited in that office. My main concern that day was asking if there was any concern with the umbilical cord wrapping around him since he was such an active baby. I felt it was legitimate since Josh had been wrapped in his and my sister had been wrapped in hers. Nothing prepared me, however, for the look on our midwife's face as she entered the room.
As the world stood still, we learned that our son had a defect in his heart. His heart. The organ that allowed the rest of his body to function. The symbol of love and unity. The center of his soul. His heart had a problem and my heart broke.

Our good midwife explained to us that there was no blood pumping through his pulmonary valve, but he was okay for now because a fetus' heart contains a shunt called the patent ductus arteriosus, or PDA, which connects the pulmonary artery and the aortic arch. This allows the heart to bypass the lungs and so the pulmonary valve is not necessary at this stage in life. The PDA generally closes itself almost immediately after birth and sort of "dissolves" in a few weeks. We discovered later that this PDA would need to be kept open by medication to keep Matthew alive until his valve could be taken care of.
Our next step was to receive a phone call from the obstetrician who oversaw our midwife. He confirmed her suspicions of the situation and set us up to see a pediatric cardiologist in Denver, CO. The week before our college finals we drove the four hours to Denver to consult with him.
Josh, my mother, and I met the pediatric cardiologist and thus began my education of the anatomy of the heart. We looked at pictures, models, and even an echo cardiogram of Matthew's heart to determine the severity of his condition. We learned the term "Pulmonary Artesia." Matthew's pulmonary valve was there but completely blocked. Unfortunately, a fetal echo cardiogram can't be 100% accurate, so we still didn't know the true extent of the complications associated with this condition except that the word "surgery" came up. The doctor hoped to be able to wait a few days after his birth to perform surgery, but he wouldn't know for sure until Matthew made his debut in the world. Suddenly that circumcision didn't seem so bad after all.
I lost a bit of my luster of life at that point. I was suddenly very afraid of my baby being born. While he was inside my belly he was safe. His constant movement reminded me that he was "alive and kicking." I couldn't be so sure of his well-being after he came out. I performed my duties as a student to the best of my ability, but I'm sure I had some extra leniency from my professors who knew all too well my circumstances. I took care of my beautiful girls the best I could, wondering if I'd have to explain to toddlers what death was. And Josh and I held each other at every chance we could. Neither of us wanted to face the possibility of the sadness that could be ours, so we immersed ourselves in each other. We prayed a lot. We called on the power of God to grant us the blessings of peace and comfort. We often felt that our son would be big, strong, and healthy, but the worry never completely dissipated.
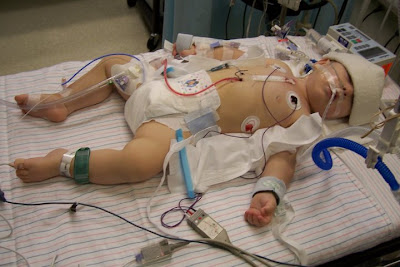
I was given the name of a woman in our area whose daughter had also had pulmonary artesia. I called and talked to her about her experience. Her daughter was now graduating from college and about to accept a position with The American Heart Association. The woman and I bonded over the worry we both felt for our children, despite the fact that our children were so far apart in age. She warned me that there would be a lot of tubes and wires surrounding Matthew after birth. She warned me that there would be tough times ahead and to keep close to my Heavenly Father. She warned me that there may be limitations placed upon my son. She also expressed love, concern, empathy, and a desire to keep us in her prayers. I never spoke to her again, but I was so glad to know that there really was someone out there, even someone in our tiny community, who knew what we were going through. Just having that knowledge lifted a little bit of our burden.
Because we lived so far from Denver, I was scheduled to be induced into labor a week before Matthew's due date. June 28, 2004, we met many of our family members at Chuck E. Cheese's in Colorado Springs to have dinner together in anticipation of my being admitted to the hospital at 8pm that evening. We happily let the girls play and rejoiced in my sister's announcement that she and her husband would be expecting their second child in 7 1/2 months. We tried to enjoy the time with our girls and the rest of our family and avoid the reality that was about to hit us in the faces: what was going to happen to our son? We arrived at the hospital and the induction began.
By the next morning, my labor was progressing, but it was much more painful than I remembered it being with the girls. I had no medication with either girl, since needles scare me. The one time I went to donate blood I was turned away because I got lightheaded and sick before any needle punctured my skin. But never the one to portray weakness, I gave birth very naturally and expected to do the same with Matthew. It didn't take long for my facade to fade and I asked for the epidural. Something wasn't right--it hurt too much. When I was eventually rushed down the hallway for an emergency c-section, more fears came to pass. Now I was going under the knife. It just couldn't be easy for us, could it?
As I had originally feared, the umbilical cord was wrapped around Matthew, suffocating him. The doctor pulled his limp body out of my belly and told the neonatal team to "Jump start this baby." Luckily, they were there waiting for us anyway because of Matthew's heart. Between the cord and Matthew's heart, I wondered if my baby had any chance of survival. Finally I got to see him for a few brief seconds before the team rushed him to the Neonatal Intensive Care Unit (NICU) to continue to check his heart. Josh felt torn between the two of us: did he stay with his wife who just underwent emergency childbirth, or did he follow his son to find out his condition. Of course I told him to go with Matthew. I was just going to be stitched up, or so I thought. Unfortunately, with the cord wrapped so tightly around Matthew, I experienced some tearing and bleeding and ended up needing a blood transfusion. It took a long time for me to get into the recovery room and even longer for me to be healthy enough to try at getting into the NICU to see Matthew up close.
When I finally made it into the NICU, I followed my friend's advice and prepared myself for the tubes and wires. There were many. I don't even know what they all were for. But it was impossible for me to hold him. I ran my finger along his cheek and spoke to him for the first time. I was asked by the nurse to stop touching him because I was exciting him too much and causing his heartbeat to rise. I forced back the tears that stung my eyes and selfishly touched him when she wasn't looking. He was my baby and I was going to provide him some sort of comfort in this new world that couldn't be comfortable for him to be thrown into. It wasn't too long before I was able to nurse him and even walk to the NICU by myself to see him. I hated the thought that he was alone, although I knew he was sleeping most of the time. I eventually got used to the idea that I didn't have to guard him 24/7 and that I should follow the old adage of Mommy sleeps when Baby sleeps.

I think it's important to warn any parent whose baby is covered in wires and tubes about the placement of IVs. I had no idea that the best place to stick a newborn for an IV was in the head. The nurses had forgotten to call me to warn me before I came in that Matthew's head would be bandaged and a huge needle-like thing would be sticking out of it. They also forgot to warn me when the second IV was placed on the other side of his head. My mother convinced me that I should take a picture of it, but I was so devastated by the whole thing that I refused to take the picture with my camera, so she took it on hers for me.
What surprised me the most about the NICU was the guilt I experienced when I saw my baby laying next to the other babies in the unit. Sometimes I felt that we didn't belong in there. Matthew grew so well in-utero that he was born 8 lbs 4 oz. He was the size of the three month old boy about to be transferred up to the Pediatric Intensive Care Unit (PICU). He looked so healthy. His feet were a bit purple, but other than that, he looked like a typical newborn. In fact, the nurses almost seemed to complain about him because when he woke up hungry, he cried. But he cried the typical newborn cry, not the mewing of a preemie. He just seemed too healthy to be there, and I felt like we were wasting the doctors' and nurses' time and energy. I had to remind myself that Matthew was known as a "cardiac baby" and he needed to be there just as much as any other baby in the unit. He still needed constant medical attention.
Shortly after birth, Matthew had his first echo cardiogram outside of the womb. The cardiologist discovered that Matthew's valve had formed almost completely. The leaflets of the valve had even formed, but they were completely sealed shut. One of our options was surgery to open the leaflets manually. Another cardiologist in the practice asked if we'd consider allowing him to perform a "procedure" rather than a "surgery." This procedure was called a Balloon Catheter Procedure and would be much less invasive. The doctor would enter one of Matthew's veins in his groin area and thread a catheter up into Matthew's heart where it would follow the flow of blood to the pulmonary valve. Once there, a special procedure would cauterize a small hole which would allow the placement of a balloon. The balloon would then expand and essentially burst open the valve to allow blood flow. I was a little skeptical of how well this would work. I worried that it would cause more damage than cure, but I knew that it may delay surgery which was the alternative if this didn't work anyway. We had to wait about four days for the proper equipment for the cauterization to come down from Toronto, Canada, along with the doctor authorized to use it. In the meantime, we watched Matthew's vitals, especially his oxygen levels. A healthy person's oxygen levels are generally between 98 - 100%, meaning they are utilizing their oxygen to the fullest extent possible. Matthew's doctor was happy to see him at 70%. However, Matthew had to have an oxygen tent (which he threw on the floor when he was three days old) and then a nasal cannula to keep him above 70%. About two weeks after birth, Matthew had his second balloon-cath (minus the fancy Canadian equipment and doctor) and his oxygen improved enough for us to take him home.

We watched Matthew grow and he seemed to have sufficient energy. He was such a laid-back baby, that we didn't realize he wasn't reaching his full potential as far as his energy level was concerned. The following December he had his third balloon-cath procedure, and then a fourth one July 2005. Because the blood had backed up so much in his heart before he was born, his muscles in his right ventricle overdeveloped and decreased the amount of space within the ventricle for blood flow. His tricuspid valve had also experienced too much strain during this time and also decreased its functionality. After the four balloon-caths, we realized that Matthew's heart wasn't repairing itself like we had hoped. The annulus which holds the pulmonary valve in place was the size it should have been when Matthew was born, not a year old. The balloon-caths kept his heart working, but didn't solve the problem. We were told that we needed to decide if we should try the balloon-cath again or just opt for surgery. Josh and I both knew that another balloon-cath was just delaying the inevitable. Our cardiologist had never needed to perform more than three balloons on a patient. It was time to face our fears.
October 12, 2005, Matthew endured his first heart surgery. The goal was to cut the annulus and place a patch to open the area for the valve so it could grow to the proper size. We expected this to be a one-time deal, however guilt never rid our lives completely. I watched Matthew lay in his hospital bed and cried knowing that I had opted for this to happen to him. It was because I gave permission that Matthew was in pain. Of course, the alternative was poor health ultimately ending in death, but it's hard to be rational when your child is hurting. Matthew seemed to recover without any problem, although Josh and I were still in school at this time. I didn't realize the commitment it would take for me to put off school, something I was very dedicated to, in order to make the several trips back to Denver when Matthew experienced too much fluid build-up around his heart. He was placed on Baby Aspirin, which didn't help, and then taken into the Cath lab once again to manually drain the fluid. When he finally recovered from the fluid build-up, he recovered very well. His energy increased and he lost the purple coloring in his feet. We expected him to be done with surgeries and that he'd just need to keep up on his check-ups as a precaution.
We were shocked to discover the following August that Matthew was not done with his heart surgeries. We had placed such high expectations on the first surgery that the prospect of a second knocked the wind out of us. The second surgery, with its surprise need was even more difficult to prepare for mentally and emotionally. However, Josh and I were becoming braver about expressing our worries and fears. We had no intention of staying in the little valley we lived in and one concern became, "If our son dies, do we bury him here and move him when we finally settle down, or do we just bury him in the area we expect to eventually settle down?" We'd never spoken aloud these types of worries and I don't know if it helped us prepare for the second surgery or if it made it more difficult to endure. The problem with the first surgery was that it was too aggressive. The leaflets of Matthew's valve now free-flowed and too much blood moved back and forth rather than pumping into the lungs. He needed a valve replacement, which meant more surgeries throughout our son's life as either he outgrew the valves or they collected too much calcium and needed replacement. Now our son was sentenced to a life of constant cardiac care. His zipper scar on his chest would be reopened every ten to fifteen years, if not sooner. This was going to require a lot more worry and prayers on my part. I wasn't sure I was up for this task.
Luckily, I had graduated from college by this time, so it was easier for me to get away for follow-up appointments. Josh and I came to Denver for the second surgery and we actually felt more comfortable in the hospital the second time around. Matt, however, slipped into a bit of a depression. It was March 2007, and Matthew lost his appetite and I couldn't get him to drink anything. We spent a few extra days in the hospital while Matthew regained some of his light back in his eyes. I was upset at seeing my two-year-old son slip into the melancholy he was in. I wondered if my depression had possibly caused his. Life wasn't supposed to be like this. I wasn't supposed to wonder about my baby's mortality. I wasn't supposed to watch three drainage tubes eject from his chest. I wasn't supposed to wander from hotel room to hospital room day and night. This wasn't supposed to happen to us. I had to quickly overcome my human emotions and portray my "strong maternal" emotions to help Matthew overcome his complacency with his situation. He had to get up and walk around. He had to eat and drink. He had to have the will to go on with life. We coaxed, we begged, we used reverse psychology, but mostly we kept ourselves in check and after five days in the hospital, Matthew came home.
Matthew still has his zipper scar and he has four belly-button sized scars from his drainage tubes along his chest. He has some small scars under his ear where his central line was placed for medication and such. But other than that, Matthew looks like your typical four-year-old boy. His last several check-ups have proven him to have a clean bill of health. We expect him to need his next surgery in about five years when his heart has outgrown his current valve, which is a bovine (cow) valve. As far as we know, Matthew will have no limitations as far as sports or other activities are concerned. He doesn't require any medication. We have tested him to find out if he may have a chromosomal defect known as 22 q11 deletion, but the test results came back normal. As far as we can tell, Matthew's heart condition is a fluke, an anomaly that will not effect his children or any of our other children. I did nothing while pregnant to cause his condition. It's taken me a long time to truly believe that. I think I've mentioned that I'm easily guilted.

I don't know that anything "inspiring" occurred with all of this except that we've made it this far. Sometimes just getting through the day is inspiring enough. Matthew loves his sisters and they love him. He knows what surgery is and that he has a special heart like Iron-Man. He's gained an empathy for children who are sick. He's a picky eater and defiantly tells me NO! just like any other preschooler. Josh and I made it through school. He's now an Emergency Room nurse and wants to focus on pediatrics once the opportunity is available. Despite the time I dedicated to my son during his times of health concern, I graduated Magna Cum Laude with my Bachelor's Degree. We lived day by day. We prayed, we were tremendously supported by our family and friends. Many people from church blessed our lives. We discovered that we are stronger people than we ever knew and our bonds as a family strengthened. I don't look forward to the future surgeries, but I know we'll make it. It's not possible for us to fail and lose faith. We've come too far as it is.

4 comments:
Thanks for sharing Shelly! My heart aches for all the worry that you went through! I am so glad that it all turned out well.
What a heartfelt post. Thank you for sharing. I can't imagine what all you and your family have endured. He is one amazing little boy and you are such an amazing mommy for being so strong.
Visiting via BPOTW.
This is an amazing story. Have you ever heard of http://awarenessbridges.blogspot.com/? I think that this post would be great for that site. There are so many parents going through all different kinds of post birth complications and it really helps to hear someone else's experience - especially when it provides so much hope.
What an amazing story.Thank you for sharing it. Your faith, no doubt, has carried you through this. He's a handsom boy!
Post a Comment